T4K3.news
TCF1 LEF1 regulate B-1a cells
New findings map how these factors sustain B-1a homeostasis and their regulatory role in inflammation

A study maps how two transcription factors regulate B-1a cells that help modulate inflammation and immune balance
TCF1 and LEF1 promote B-1a cell homeostasis and regulatory function
A new study shows that the transcription factors TCF1 and LEF1 are key regulators of B-1a cells, a subset of innate like B cells. The research finds LEF1 is most active in fetal and bone marrow B-1 progenitors while TCF1 is higher in mature splenic and peritoneal B-1 cells. Mice lacking both factors have fewer B-1a cells and poor maintenance of this population. The loss also disrupts a MYC driven metabolic program and reduces the cells stem like features after activation, partly through IL-10 production. When TCF1 and LEF1 are absent, B-1a cells proliferate too much and enter an exhausted state with lower IL-10 and PD-L1 expression. In functional tests, transfer of B-1 cells missing these factors fails to suppress inflammation in the brain. The work also notes that TCF1 and LEF1 are expressed in human chronic lymphocytic leukemia B cells and in a B-1 like population found in pleural fluid and blood of some patients with pleural infection. The team used mouse models, including conditional knockouts and chimeras, along with advanced sequencing and cell profiling to map the transcriptional program that links self renewal with regulatory capacity.
Key Takeaways
"TCF1 and LEF1 steer a stem like program in B-1a cells"
core mechanism
"Without TCF1 and LEF1 B-1a cells exhaust and lose IL-10"
knockout outcome
"Human pleural B-1 like cells show the same handprint"
human relevance
"A transcriptional duo reshapes how we view immune regulation"
editorial takeaway
The findings add a new layer to how immune regulation is wired at the transcriptional level. They show a clear link between stem like properties and regulatory function in a single B cell subset, controlled by a shared TCF1 LEF1 program that can shift cell fate on activation. The human relevance is intriguing, especially in diseases where B cells influence inflammation, but translating these results to therapies will require caution. Differences between mouse models and human B-1 cell biology mean any clinical promise is years away. Still, the study points to a potential axis for tuning immune responses in infections and autoimmune conditions while highlighting the importance of maintaining balance in B-1a cell activity.
Highlights
- TCF1 and LEF1 steer a stem like program in B-1a cells
- Without these factors B-1a cells exhaust and lose IL-10
- Human pleural B-1 like cells show the same handprint
- A transcriptional duo reshapes how we view immune regulation
Ethical and translational considerations
The study involves human samples and animal work. Translating findings to therapies will require rigorous ethical oversight and clear communication about potential risks and benefits. Privacy and consent for human tissues must be maintained as studies move toward clinical relevance.
As science maps immune control, practical applications will require careful, patient led development
Enjoyed this? Let your friends know!
Related News
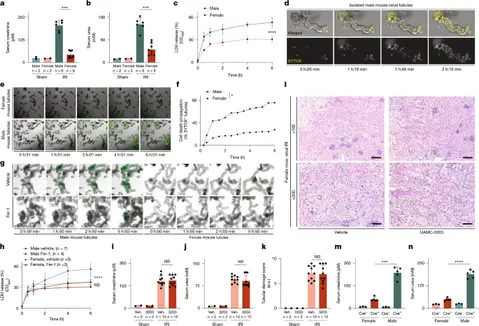
Estrogen protects kidneys from ferroptosis

Kidney Proteomics Maps New Targets for CKM health
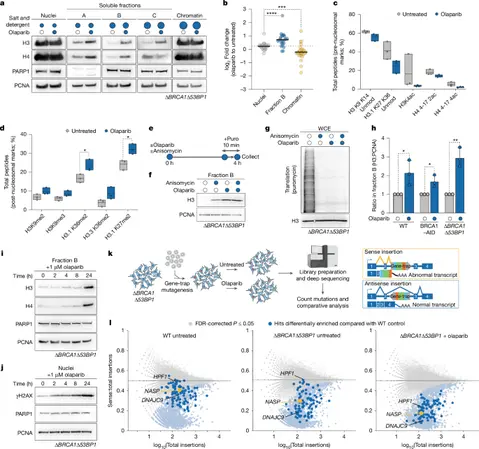
NASP histone turnover ties PARPi resistance

NAD Plus prompts scrutiny over ageing claims

Dietary Changes Could Help Reduce Headaches

Pharmacists warn about coffee and supplements

Potato guide changes how we think about fries

Research links tattoos to increased cancer risk
