T4K3.news
Mortality gap data update
A new analysis shows rising death rates among young Americans compared with peers in rich countries.
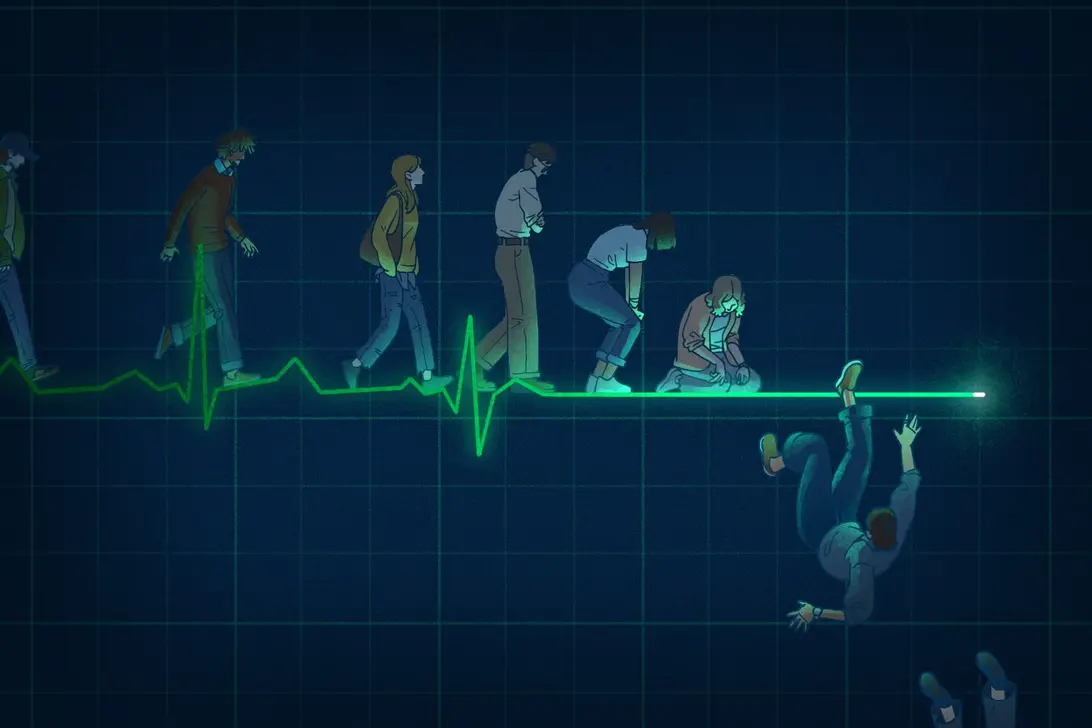
A data driven look shows Americans born in the 1980s and 1990s face higher death rates than peers in other wealthy nations.
U.S. millennial mortality gap widens beyond peers
A new analysis shows that mortality among Americans born in the 1980s and 1990s is higher than in peers across other wealthy nations. The United States sees about 3 million deaths each year, and among people under 65 the gap is large. In 2023 roughly 700,000 deaths could have been avoided if the U.S. matched death rates in peer countries. For ages 25 to 44 the gap is about 62 percent, and early adults are 2.6 times more likely to die than their counterparts in other rich nations.
Experts say the picture is broader than one crisis. The pandemic amplified some trends but did not start them. The early adult group faced rising deaths from drug overdoses, car crashes, digestive diseases, and diabetes, alongside ongoing issues like homicide and circulatory disease. By 2023 the chance of dying for early adults was 70 percent higher than it would have been if old trends continued, and this pattern is not easily explained away by COVID alone. Some researchers point to deindustrialization, weak social safety nets, and gaps in health care as part of the mix, while others highlight cultural and behavioral factors. The piece notes that policy choices after 2020 may influence these trends for younger workers and families, and that more work is needed to untangle causes.
Key Takeaways
"America becomes a deadly place for people in their 20s and 30s"
tweetable reflection on young adults risk
"A safety net that does not keep pace is a life and death policy choice"
policy critique with real world impact
"Invest in millennials and Gen Z or pay the cost in lives"
policy argument for investment
"The price of neglect shows up in rising death rates"
editorial observation
The data point to a structural problem rather than a single cause. The mortality gap cuts across multiple illnesses and injuries, suggesting that health outcomes are tied to the broader environment—jobs, housing, income security, and access to care. In other words, improving death rates for younger Americans likely requires coordinated changes across health policy, labor markets, and social supports. The analysis also frames the issue as a generational challenge with long term political and economic consequences, not just a health statistic.
Looking ahead, policymakers face a test. If the United States wants to keep its workforce and civic life healthy, it must address how the safety net fits the realities of millennial and Gen Z life cycles. Without stepped up investment in education, housing, and affordable care, the mortality gap could persist or widen, reshaping the country’s future more than any one election cycle.
Highlights
- America becomes a deadly place for people in their 20s and 30s
- A safety net that does not keep pace is a life and death policy choice
- Invest in millennials and Gen Z or pay the cost in lives
- The price of neglect shows up in rising death rates
Mortality gap tied to budget and political risk
The piece links rising early adult deaths to safety nets and policy choices, a topic that may trigger political backlash and budget scrutiny.
What happens next will test whether policy can bend this grim trend.
Enjoyed this? Let your friends know!
Related News

Police will share suspects ethnicity and nationality
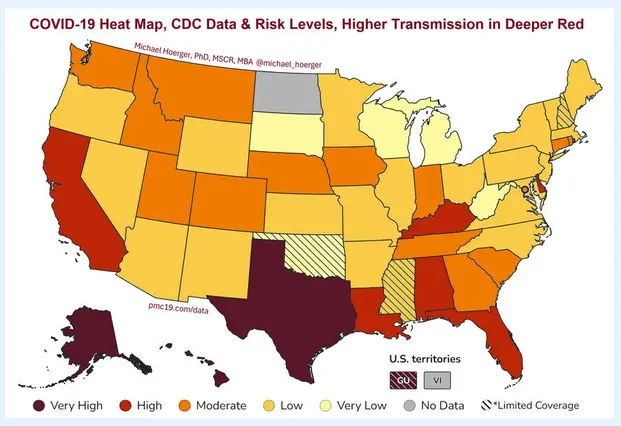
Covidwave update prompts health guidance

Red Bull Racing struggles with performance at the Hungarian GP

MTD ITSA expands to self-employed and landlords
FEWS NET Back Online
New study links walking 9000 steps daily to lower cancer risk

Gmail users urged to change passwords urgently

Covid vaccine update timeline