T4K3.news
NHS dentistry under strain
Rising misdiagnoses and payouts spotlight pressure on NHS dentistry and patient safety

An analysis of rising misdiagnoses in NHS dentistry amid staffing shortages and growing compensation payouts to patients.
NHS dentistry strain drives misdiagnoses and rising payouts
Saira Malik, a civil servant in Surbiton, spent nearly a decade at the same NHS dental practice before a sequence of missed signs led to serious harm. Beginning in 2016 with toothache, she was repeatedly told there was no decay, only to learn later that untreated decay had progressed. In 2019 a tooth extraction at a different clinic became a painful turning point when a piece of bone and a blood vessel were torn away, leaving her in intensive care. Her story underscores how a missed diagnosis can escalate into life threatening complications and long-term fear of dental care.
Data shows a broader pattern: NHS Resolution reports a 50 percent rise in payouts for dental procedure mistakes over five years, totaling £11 million, with many cases arising in local practices rather than hospitals. Law firms also note a doubling of misdiagnosis claims in the same period, and a year-on-year rise in botched surgeries since 2020. The roots of the problem appear tied to a nationwide shortage of NHS dentists, with England counting about 23,000 dentists – down 1,100 from pre-pandemic levels. About 95 percent of practices are not accepting new NHS patients, tightening access and raising the stakes for preventive care.
Key Takeaways
"The errors are unfortunate, and still rare."
Dr Abhi Pal on frequency and reporting gaps in dental negligence cases
"The reality of that is the longer someone has to wait, the more drastic the treatment becomes"
Dr Jeffrey Sherer discussing how delays worsen outcomes
"We have seen a huge rise in cases over recent years"
Chris Dean of the Dental Law Partnership on rising claims
"If this happens to you, it’s possible that your dentist has missed something"
Advice to patients from a legal expert
The situation points to a health system under pressure, where staffing gaps and funding gaps meet rising patient expectations. A lack of mandatory reporting on misdiagnoses makes it hard to gauge true scope, so harm may be undercounted. As wait times grow, routine care can turn into complex, costly interventions, which in turn fuels a cycle of complaints and lawsuits. The sector has acknowledged the problem, but policy moves so far have not reversed the trend, leaving patients exposed and clinicians stretched. In short, funding, access and accountability must align to reduce preventable harm.
Highlights
- When waiting stretches, simple fixes become major operations
- Prevention saves more than a root canal
- A wait list should never become a life risk
- Care slipping under pressure hides a larger failure
NHS dentistry strain risks patient harm
The piece highlights budgetary and staffing pressures in NHS dentistry, rising compensation payouts, and potential public backlash. These factors create sensitive, politically charged terrain for reform.
Policy makers should listen to patients and dentists before the next patient is rushed into costly surgery.
Enjoyed this? Let your friends know!
Related News

Back pain affects millions globally
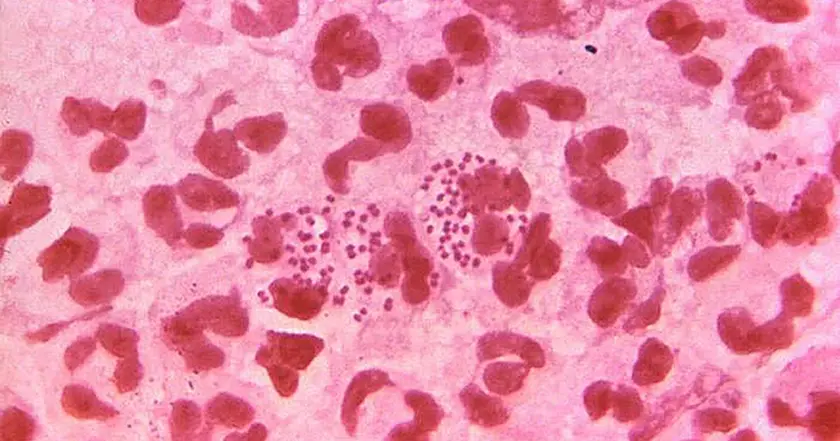
Bolton and Bury launch gonorrhoea vaccine program

UK launches gonorrhoea vaccine rollout

Cancer care funds at risk for UK patients

Vicky Pattison reveals struggle with misdiagnosis

New NHS guidance on fat jabs issued

NHS heat related deaths spark cooling debate

AstraZeneca's future in UK at risk due to NHS pricing policies
