T4K3.news
Increased early stage colon cancers reported in younger adults
More screenings for adults aged 45-49 lead to early stage diagnoses of colon cancer, research finds.

New findings show more early stage colon cancers in younger adults linked to increased screening.
Early stage colon cancers increase in those aged 45-49 due to higher screening rates
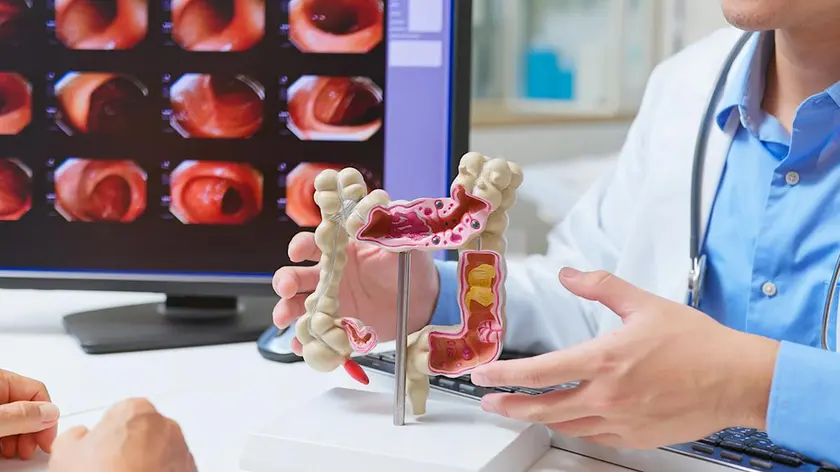
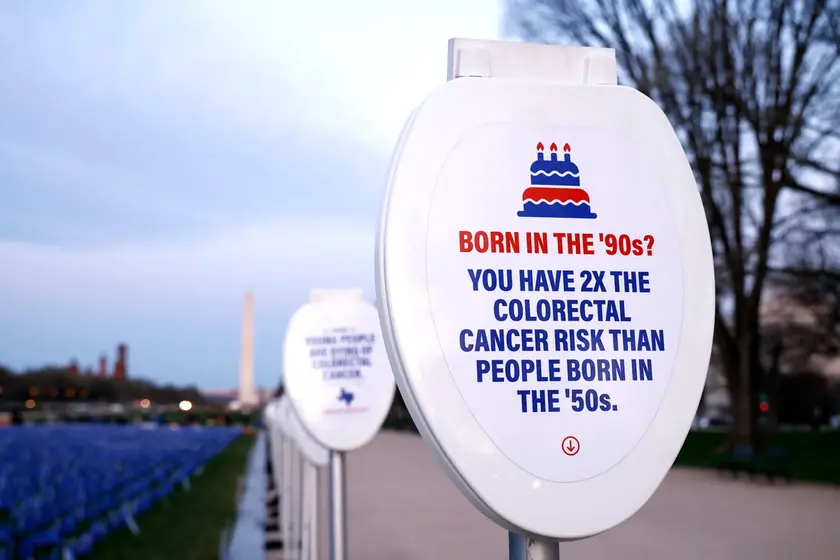
New research from the American Cancer Society indicates that more screenings among adults aged 45 to 49 are resulting in increased early stage colon cancer diagnoses. The studies, published in the Journal of the American Medical Association, reveal a significant uptick in both screenings and diagnoses since guidelines lowered the recommended age for colorectal screenings from 50 to 45. From 2019 to 2023, screenings in this age group rose by 62%. Researchers, including lead authors Elizabeth Schafer and Jessica Star, emphasized the importance of these findings but also highlighted the need for improved equity in screening access, which remains a concern.
Key Takeaways
"The uptick of cases is likely due to first-time screening in the wake of new recommendations for younger average-risk adults to begin testing for colorectal cancer earlier."
This highlights the positive effect of raising awareness about early screenings for colorectal cancer.
"Screening for colorectal cancer in ages 45-49 remains suboptimal and has not increased equitably by both education attainment and insurance status."
This reflects the ongoing disparities in healthcare access that need to be addressed.
"A change would greatly damage all the work we've done in preventative care, making people sicker, and driving up costs and premiums."
This emphasizes the potential negative ramifications of policy shifts regarding healthcare recommendations.
"This is extremely concerning — and doing the opposite of making America healthy."
This statement underscores strong apprehensions about the future of public health initiatives under changing leadership.
The rise in early stage diagnoses is promising but reveals deeper issues in healthcare access and equity. Despite recommendations for earlier screenings, many adults, especially those with lower educational attainment or poor insurance status, still face barriers to effective screening. This discrepancy could lead to long-term health problems that the current increase in screenings cannot resolve alone. The potential removal of Task Force members raises additional fears about the future of preventive healthcare, likely affecting public health outcomes and leading to increased treatment costs.
Highlights
- More screenings mean more early stage diagnoses.
- Equity in healthcare is essential for effective cancer prevention.
- Rising diagnoses indicate a need for better screening access.
- Preventive care changes may cost lives if not handled carefully.
Concerns over healthcare access and policy changes
New recommendations might be jeopardized by political decisions, potentially worsening health outcomes.
The findings indicate a critical moment for public health strategies that require immediate attention.
Enjoyed this? Let your friends know!
Related News
Colorectal cancer rises in younger adults as screening guidelines expand

Early screenings rise among 45 to 49
Rising cancer rates in young women

Young Americans face higher rectal cancer risk

Colorectal cancer screenings expand as cases rise
Colorectal cancer rates soar among young adults

Victoria Collins diagnosed with stage three bowel cancer at 40
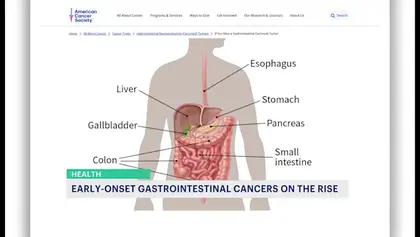
Increase in gastrointestinal cancer cases among young adults reported
