T4K3.news
Gene edited cells enable insulin production without immunosuppressants
A patient with type 1 diabetes produced insulin from edited donor cells without immune drugs in a preliminary study.

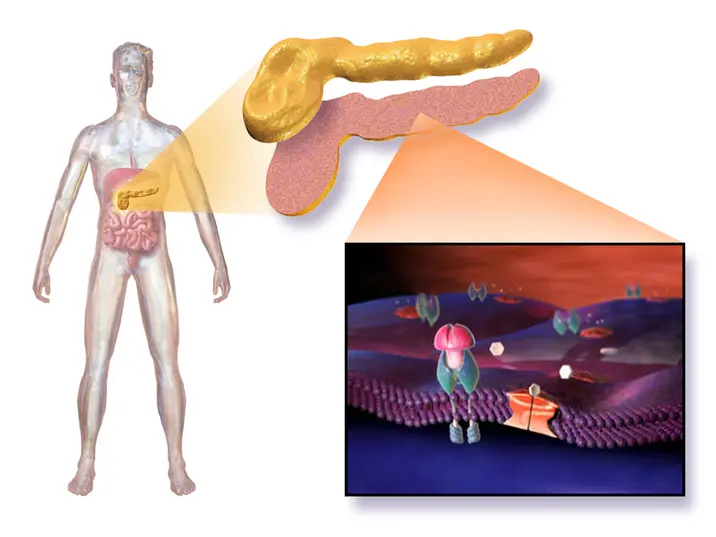
A proof‑of‑concept study shows donor islet cells edited to avoid immune rejection can produce insulin without lifelong immune drugs in a type 1 diabetes patient.
Gene edited pancreatic cells enable insulin production without immunosuppressants
A team of researchers from Sweden and the United States published findings in the New England Journal of Medicine about a 42‑year‑old man with long‑standing type 1 diabetes. Donor islet cells were genetically edited to reduce immune recognition and increase immune protection, allowing the patient to produce insulin without immunosuppressive therapy. In the months after the transplant, fully edited cells continued to function and were not rejected by the patient’s immune system, though some edited cells failed and were cleared. The patient experienced non serious adverse events, none tied to the transplanted cells, and insulin production appeared sustained at about 12 weeks.
The study is described as a cautious step toward immune‑evasive transplantation rather than a demonstrated cure. While early results are encouraging, the dose given was small and durability over time remains unknown. If future trials confirm safety and long‑term function, this approach could lessen or eventually remove the need for lifelong drugs that blunt immunity, a major drawback of current islet cell therapies.
Key Takeaways
"Our study, although preliminary, suggests that immune evasion is an alternative concept for the circumvention of allorejection"
Researchers describe immune evasion as a key idea behind the method
"If these edits prove durable, the need for immunosuppressants could shrink"
Editorial take on future implications
"The surviving cells produced insulin as normal"
Direct observation from the trial
"This could revolutionize how we treat chronic diseases that rely on transplantation"
Broad implications for medicine
The case signals a potential shift in how we think about transplantation for diabetes. Immune‑modulation by gene editing could reduce the burden of immunosuppression, improving quality of life and reducing infection risk. Yet the road to widespread use is long: questions about long‑term safety, potential off‑target edits, and the therapy’s effectiveness in a broader patient group must be answered before considering clinical practice changes. The findings also invite a broader debate about how far gene editing should go in living patients and how to regulate such therapies without stifling innovation.
Highlights
- Immune evasion could change transplant medicine
- A proof of concept that questions the need for lifelong drugs
- Durability and safety will decide the path forward
- Edited cells may redefine what a cure for diabetes looks like
Further trials will determine whether this is a durable path toward a true cure.
Enjoyed this? Let your friends know!
Related News
First gene-edited islet transplant succeeds

Study shows promise for type 1 diabetes treatment

Study reveals microglia regulate GABAergic neurogenesis

Groundbreaking oat research promises robust crop production

Common virus linked to increased MS risk in Americans

Experts warn cancer causing chemicals threaten humanity

Breakthrough Discovery in Diabetes Treatment Unveiled

Study reveals human DNA linked to hibernation
