T4K3.news
UnitedHealth under investigation by Justice Department
UnitedHealth discloses DOJ investigation into its Medicare billing practices, facing serious scrutiny.

UnitedHealth is under investigation by the Justice Department for its Medicare billing practices.
UnitedHealth faces scrutiny from Justice Department over Medicare practices
UnitedHealth Group disclosed a Justice Department investigation into its Medicare billing practices, as detailed in a recent securities filing. The company is responding to formal criminal and civil requests from the DOJ and has initiated a third-party review of its business operations. This follows earlier reports of potential Medicare fraud, where the DOJ has been gathering evidence, including interviews with doctors about UnitedHealth's billing techniques. Despite these challenges, UnitedHealth maintains confidence in its practices, claiming audits affirm its policy accuracy. This investigation underscores a turbulent period for the healthcare giant, which has faced significant financial and leadership challenges in recent months.
Key Takeaways
"UnitedHealth has full confidence in its practices and is committed to working cooperatively with the Department throughout this process."
This statement reflects UnitedHealth's position amid the ongoing investigation and their willingness to comply.
"The DOJ is conducting a criminal investigation into the health-care giant over possible Medicare fraud."
This highlights the severity of the scrutiny facing UnitedHealth, marking a significant challenge for the company.
The investigation by the DOJ adds another layer of complexity to UnitedHealth's operations, particularly as the Medicare Advantage program is crucial to its revenue. The scrutiny reflects broader systemic issues within the healthcare sector, where accountability for billing practices is increasingly being called into question. As healthcare costs rise and profitability becomes more challenging, companies must navigate a fraught landscape of compliance and public perception. Furthermore, the confidence expressed by UnitedHealth, juxtaposed with its declining stock performance, highlights the tension between corporate claims and investor skepticism. In a time when healthcare funding is under intense scrutiny, the outcomes of this investigation could significantly impact not just UnitedHealth, but the entire industry.
Highlights
- UnitedHealth faces a DOJ investigation over its Medicare practices.
- Claims of fraud cast a shadow on UnitedHealth's practices.
- Confidence in billing practices meets federal scrutiny.
- A turbulent year for UnitedHealth raises serious concerns.
Investigation raises concerns for UnitedHealth
The ongoing Justice Department investigation into Medicare billing practices poses significant risks for UnitedHealth, potentially impacting investor confidence and regulatory scrutiny.
As investigations continue, the impact on UnitedHealth's future operations could be significant.
Enjoyed this? Let your friends know!
Related News

UnitedHealth faces federal investigation regarding Medicare practices
:max_bytes(150000):strip_icc()/GettyImages-2227230951-271d713fa8f046b89e6677f0a933fb76.jpg)
UnitedHealth Group to Report Second Quarter Earnings Soon

UnitedHealth Faces Federal Investigation

UnitedHealth to report Q2 earnings amid investigation

UnitedHealth Stock Declines Despite Strong Earnings

UnitedHealth Group announces disappointing Q2 2025 earnings guidance
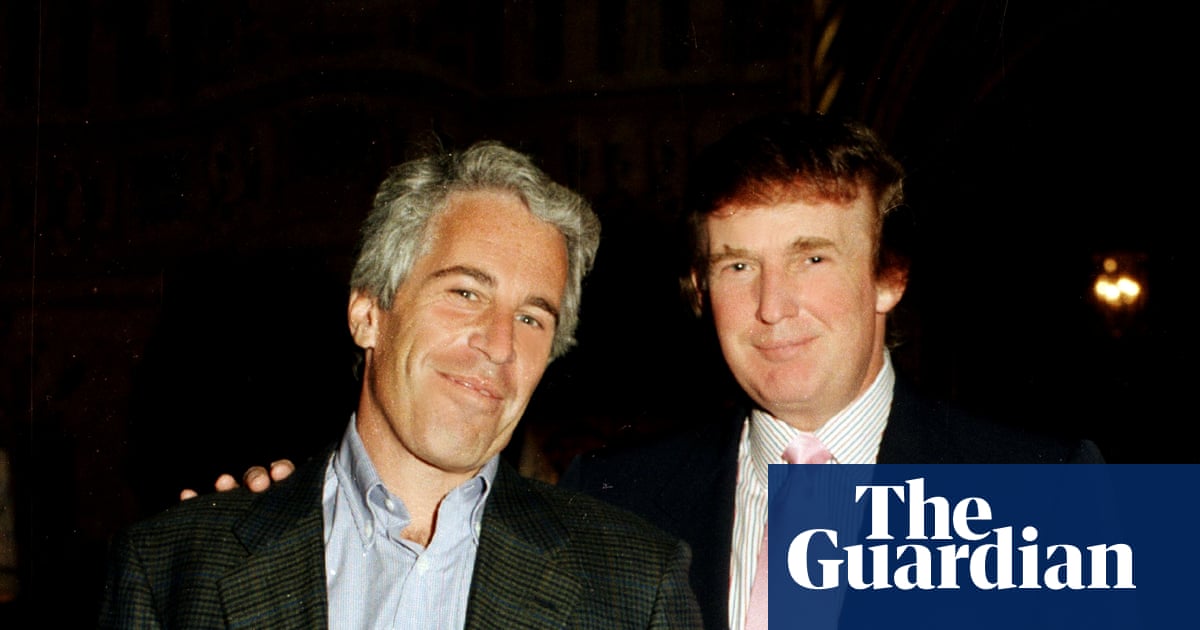
Trump linked to Epstein files by Justice Department

Investigation launched into Jack Smith by Special Counsel
