T4K3.news
Unexplained arm bruising prompts medical review
A reader with new bruising that bleeds should see a GP for evaluation.

A health columnist analyzes a reader’s case of new arm bruising that bleeds, urging medical evaluation for possible underlying conditions.
Unexplained arm bruising prompts medical review
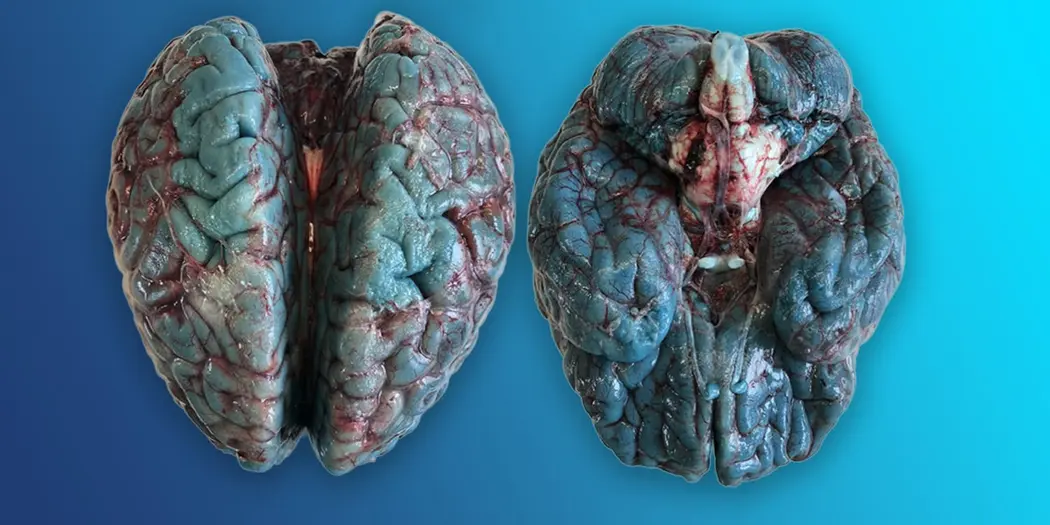
A 60-year-old man noticed bruise-like marks on the right forearm for about a year. He has a known B12 deficiency and COPD. A nurse who gave a B12 injection told him the spots were a sign of skin aging. In recent months the marks sometimes bleed. The reader asks whether to see a GP. The clinician notes a reticular, or net-like, bruising pattern on the lower arm with some scab formation. The doctor advises a GP visit and suggests sharing images via an online consultation to prepare for the appointment. A range of conditions could be considered, including vasculitis, a clotting disorder, or autoimmune diseases such as lupus. Any abnormal bruising and bleeding should always be checked.
Key Takeaways
"Any abnormal bruising or bleeding should always be checked out"
Dr Zoe Williams' guidance to patients
"The short answer is yes you should see a doctor"
Direct advice to the patient in the article
"Protect yourself by sticking to main pathways in green spaces after a walk"
Lyme disease prevention guidance
"Lyme disease peaks in summer"
Seasonal risk reminder
Dismissing new bleeding bruises as aging is a common pitfall in primary care. This case shows why a careful eye on visible signs matters, especially with age and chronic illness. A reticular bruising pattern is not a single clue; it invites blood tests and possibly a specialist review. The presence of B12 deficiency and COPD can affect how symptoms are read, so doctors must separate routine aging from possible vascular or autoimmune issues.
Public health messaging about Lyme disease is important but must stay clear and proportionate. The piece links a personal health concern with a seasonal risk, reminding readers to check for ticks after outdoor activity. Online tools such as e consult can help patients prepare for a visit, yet nothing replaces a physical examination when bleeding is involved. The broader trend is toward proactive patient engagement and informed reassurance rather than quick, generic advice.
Highlights
- Listen to small signs before they become big problems
- Bleeding bruises deserve a medical check not silence
- Health care starts with listening before labeling
- Pictures shared ahead of a visit can speed up answers
Health signs matter more than age when it comes to medical care
Enjoyed this? Let your friends know!
Related News

Fort Stewart Shooting Suspect Identified

Quentin Johnston concussion prompts Chargers to review return to play protocol
Blue brain discoloration tied to medical dyes identified
Rising cancer rates in young women
Escalator tragedy prompts safety review

Australian man faces advanced lung cancer complications

Arizona child abuse tragedy prompts protection system review

Persistent sore throat may signal cancer
