T4K3.news
Lab grown spinal cord transplant heads toward first human trial
Israeli researchers prepare for compassionate-use trials after strong animal results

Tel Aviv University researchers move from animal tests to a compassionate-use human trial for lab-grown spinal cord tissue to help paralyzed patients walk again.
Lab grown spinal cord transplant heads toward first human trial
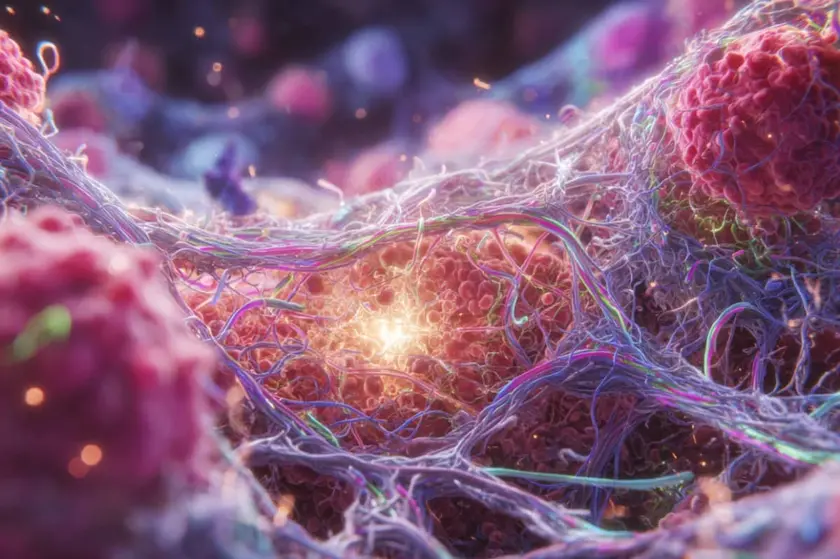
Tel Aviv University researchers led by Prof. Tal Dvir have advanced their project from animal work to a planned human trial. After years of development, the team says a 3D, lab-created spinal cord tissue can be implanted at the injury site and may restore communication between the brain and affected limbs. Animal studies reported that more than 80% of subjects with chronic injuries recovered the ability to walk. The Health Ministry has granted compassionate-use approval for eight patients, with the first Israeli patient expected to be treated soon. The early stage targets injuries that are less than a year old, offering a path to measure safety and initial effectiveness before broader use.
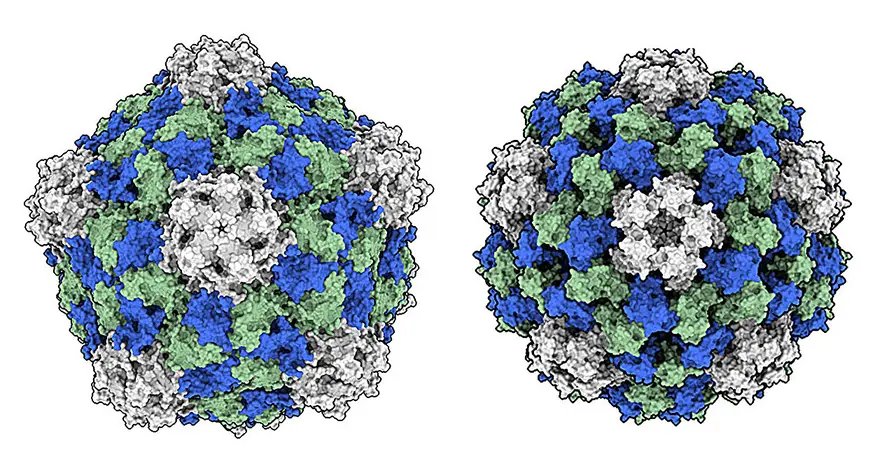
The approach combines patient-derived cells reprogrammed into stem cells with a personalized gel made from the patient’s fat tissue. The finished tissue is designed to integrate with the existing spinal cord, bridging damaged segments and allowing signals to pass again. The researchers emphasize that immune rejection is a major hurdle, so the method centers on autologous cells to minimize rejection and maximize compatibility. A key goal is to create a transplant that behaves like real spinal tissue rather than a simple implant, which would require careful fusion with the body's neural network.
Key Takeaways
"The goal is to build a small piece of spinal cord that behaves like the real thing"
Dvir explaining how the implant should function in the body
"We take blood cells from the patient and reprogram them into stem cells"
Autologous cell approach to avoid immune rejection
"This could help all patients with paralysis"
Dvir on the broader potential of the technology
"The spinal cord is like an electric cable and must reconnect for signals to pass"
Explanation of the science behind the challenge
This progress could redefine recovery for spinal injuries, but it also comes with long odds. Translating a lab model into human benefit will hinge on safety, ethical oversight, and the ability to scale production for diverse injuries. Even if the first patients respond well, researchers acknowledge that many people differ in the timing and location of injuries, which will shape who can benefit and when. The move to compassionate-use trials signals regulatory guardrails are in place, yet public expectations will rise quickly if early results look promising.
Highlights
- Autologous cells reduce the risk of rejection and boost compatibility
- We aim to build a spinal cord that behaves like the real thing
- The first Israeli patient marks a milestone in regenerative medicine
- This is a long road with many tests ahead
Progress in the lab invites cautious optimism and steady oversight as the path to real-world impact unfolds.
Enjoyed this? Let your friends know!
Related News
Body quirks draw online attention

Police will share suspects ethnicity and nationality

Israeli Forces Face Allegations of War Crimes

Longevity reshapes the federal budget reality
Plant virus shows potential in cancer therapy
Video game prequels redefine the series

Tooth Regeneration Moves Toward Trials
CAPPSID shows promise for cancer therapy
