T4K3.news
Health guidance collisions with eating disorder recovery
A writer shares how cholesterol care and weight stigma intersect with personal recovery, urging more nuanced health guidance.

A writer explains how medical guidance to lower cholesterol clashes with recovery from anorexia, revealing flaws in today’s health messaging.
Health Advice Collides With Eating Disorder Recovery
Amelia Tait recounts a journey from adolescent anorexia to a 2024 diagnosis of very high cholesterol. After years of restriction, she describes a lifestyle that swung between indulgence and danger, ultimately prompting a half‑year shift to a lower saturated fat diet and a move back toward normal cholesterol levels. The piece notes that the Our Future Health screening in 2023 first alerted her to cholesterol problems and that a six‑month effort reduced risk factors.
The broader critique centers on health messaging that equates health with weight. She recalls a dismissive doctor response, a nurse’s note banning fancy breads, and calories creeping into health apps that reappear even after recovery. The author argues that healthy living should focus on nutrition quality and cardiovascular risk, not a fixed calorie count or a thin ideal. She warns that society’s default assumption is that healthier living means shedding pounds, a trap that can pull someone back toward disordered thinking and behaviors.
Key Takeaways
"Treats are not something that have to be earned"
From the author’s assertion about reframing indulgence
"Being told to monitor calories felt like inviting me back to my disorder"
Statement about how certain tools can trigger relapse
"The number on my blood test results matters more than the number on the scale"
Point about medical data over appearance
"The world told me the scariest consequence of eating what you liked was gaining weight"
Comment on societal pressure and weight stigma
The piece foregrounds a tension many readers recognize: the clash between personal healing from an eating disorder and a medical system that still relies on weight as a primary signal of health. It argues for nuance in nutrition guidance, highlighting that high‑calorie foods can be nutrient dense and that low‑calorie labels do not guarantee health. It also calls out weight bias in clinical settings, suggesting doctors should tailor advice to medical risk rather than body size alone. The editorial implies a need for compassionate, individualized care that centers bodily health markers beyond the scale and avoids retraumatizing patients.
Looking ahead, the article pushes policymakers and clinicians to rethink public health messaging. It proposes clearer education on how cholesterol and fat intake affect heart risk, without framing every dietary choice through the lens of weight. The hope is a system that supports mental health while reducing cardiovascular risk, rather than a simplistic diet culture that still dominates many conversations about health.
Highlights
- Treats are not something that have to be earned
- Being told to monitor calories felt like inviting me back to my disorder
- The number on my blood test results matters more than the number on the scale
- The world told me the scariest consequence of eating what you liked was gaining weight
Health guidance risks for eating disorder history
The article shows how health messaging tied to cholesterol and diet can retraumatize people with eating disorder histories and reinforce weight bias in clinical settings.
Health guidance works best when it respects lived experience and centers real medical risk.
Enjoyed this? Let your friends know!
Related News
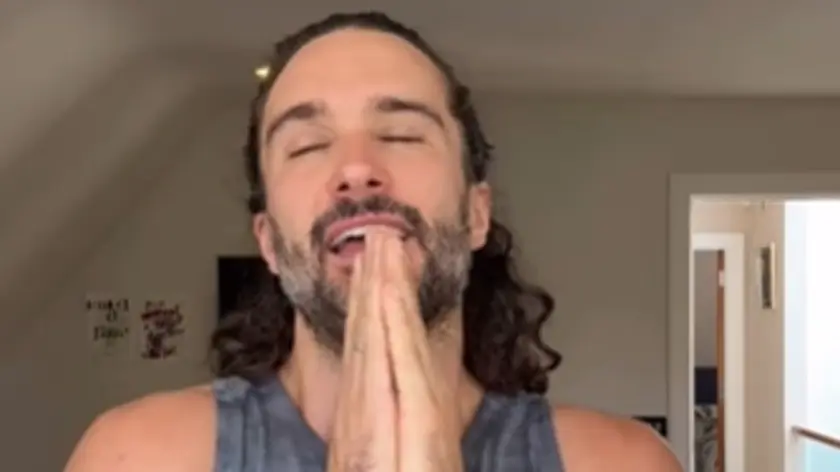
Wicks faces health messaging backlash

Weight-loss drugs linked to increased eating disorders in the US
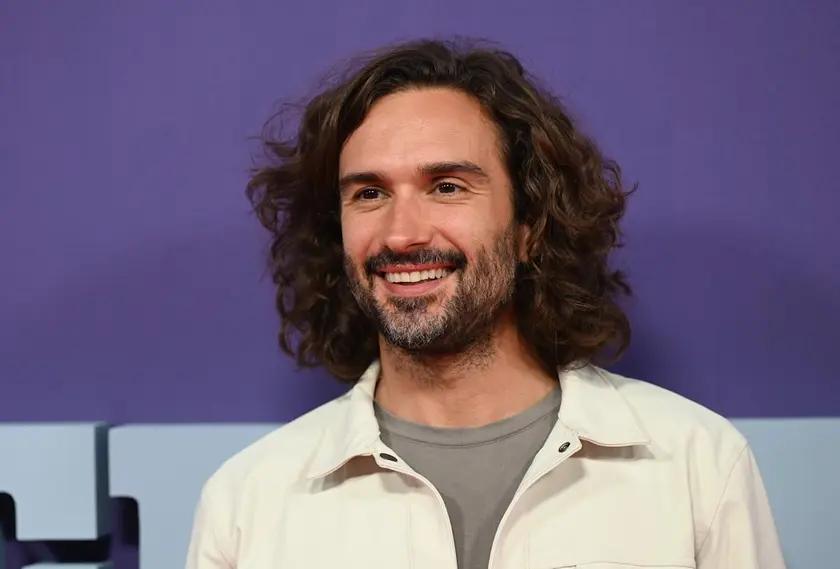
Health experts weigh in on Wicks sugar guidance

Balanced view on kids and fast food

Chloe Cherry opens up about eating disorder

Teenage girl dies from starvation due to NHS failures

Family faces horror after hotel buffet meal in Gran Canaria

Gut health alert 11 foods tied to diarrhea
